An unusual localization of intraosseous schwannoma: the hamate bone
Abstract
Intraosseous
schwannoma of the hamate bone presented in this case is a very rare benign
tumor, and its diagnosis com[1]bined
with clinical, imaging and needle biopsy is important to guide further therapy.
The diagnosis of schwannoma of the hamate was proved histologically following
its surgical treatment by curettage.
Introduction
Schwannomas
(neurilemmomas) are the most common tumors derived from schwann cells of nerve
fibers. It is a rela[1]tively
common tumor, approximately 5% of all benign soft tissue tumors. Intraosseous
schwannoma, however, is very rare, accounting for less than 1% of all benign
bone tumors.1-8 They are generally aympto[1]matic. Radiologically,
schwannomas pres[1]ent
as well-circumscribed lytic, expansile intramedullary lesions with sclerotic
bor[1]ders.
There is no predilection of sex, age and location. There is no case of
intraosseous schwannoma around the wrist has been described in literature. We
present the first case report of an intraosseous schwannoma of hamate bone of
the wrist.
Case Report
A
34-year-old woman presented with 2- year history of the right wrist pain. The
pain generally occured in the morning and increased with daily activations.
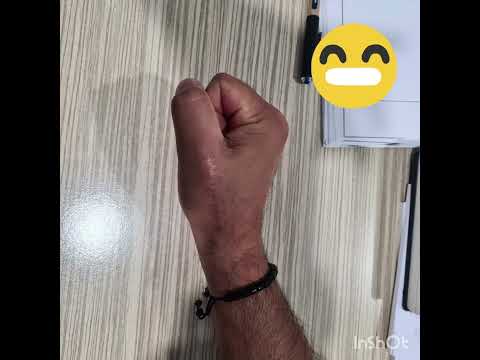
There was mildly significant swelling on the wrist. Physical examination showed
a 2×2-cm firm, round and hard mass on the dorsal aspect of the right wrist. The
wrist had almost full range of motion. The overlying skin was intact, and there
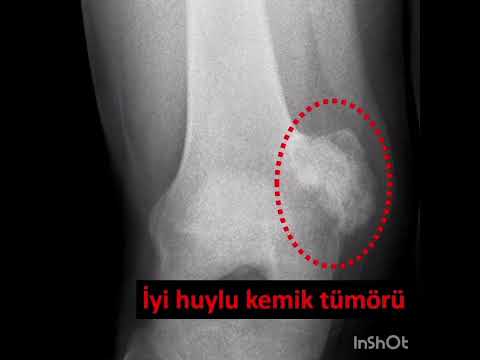
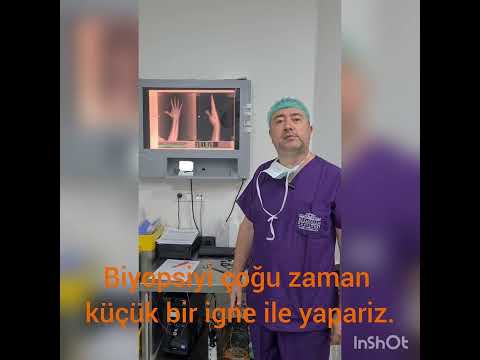
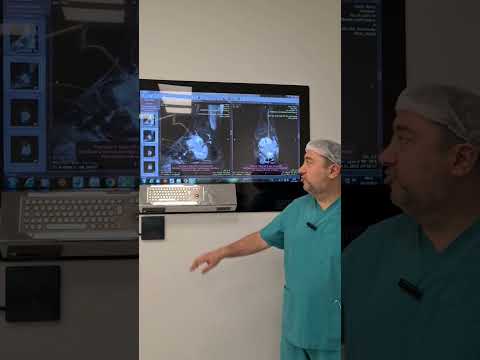
was no evidence of wamth, erythema, or induration. Plain radiographs revealed a
lytic lesion with well-defined sclerotic borders in the hamate bone. It was
multilocular, with no inner calcifications; the dorsal cortical part of the
bone was disrupted without periosteal reaction (Figure 1A). Computerized tomog[1]raphy
(CT) scans showed the lesion was expansile with cortical break-through in its
its dorsal aspect. It has sclerotic, well[1]defined borders with narrow
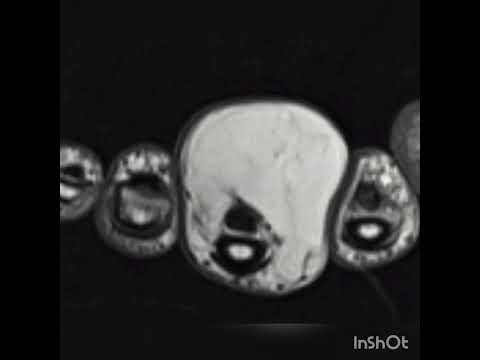
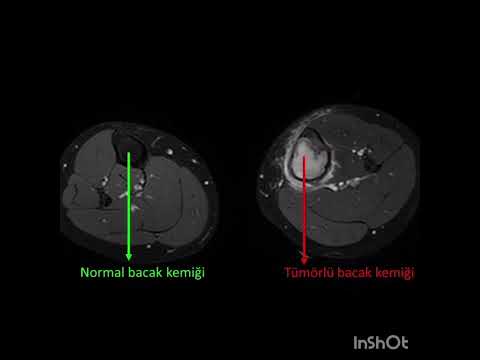
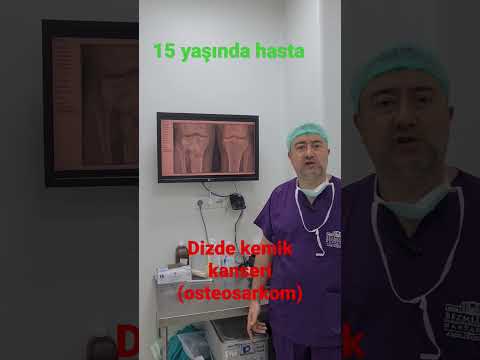
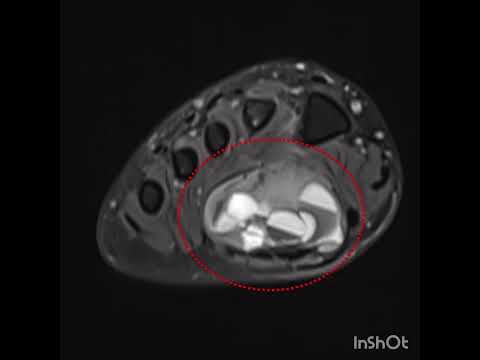
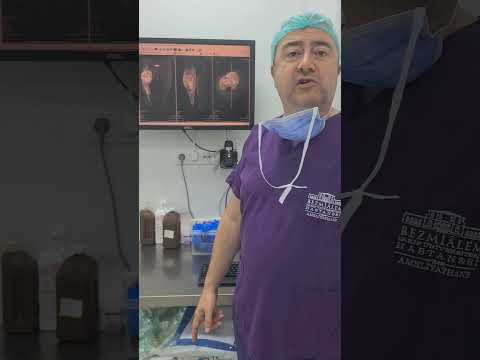
transition zone (Figure 1B). Magnetic resonance imaging (MRI) revealed again
cortical disruption of the dorsal cortex and extraosseous soft tis[1]sue
extension of the lesion to the dorsal side of the hand (Figure 2A). The lesion
was hyperintense on PD-weighted sequences, and demonstrated solid and
homogenous enhancement on contrast-enhanced T1- weighted sequences. Despite its
soft tissue extension, it has still well-defined borders within bone and soft
tissues. Immunohistochemistry studies of the tissue obtained by a needle biopsy
showed S-100 protein positive spindle cells, addressing a benign neurogenic
tumor. Then, we per[1]formed
totally resection of the lesion by curettage via dorsal longitudinal incision.
After curettage, bone defect was recon[1]structed
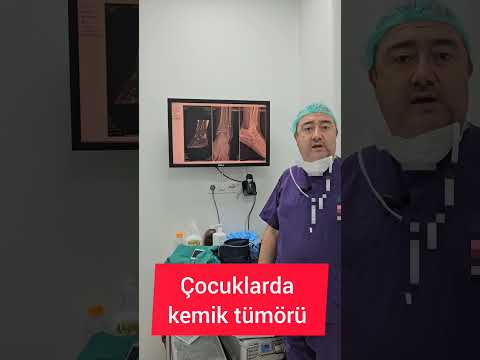
by autograft harvested from the iliac crest. The gross specimen showed a solid
lobular tumor with clear boundary, partly located within the bone. Histolo -
gically, the tumor was composed of multi[1]ple nodules of spindled
Schwann cells with[1]in
the bone parenchyma (Figure 3A and B). Antoni A pattern was predominant.
Nuclear palisading and Verocay bodies were present (Figure 3C). Immunohi
stochemically, tumoral cells were strongly positive for S[1]100
protein (Figure 3D). The final diagnosis was plexiform schwannoma of the bone.
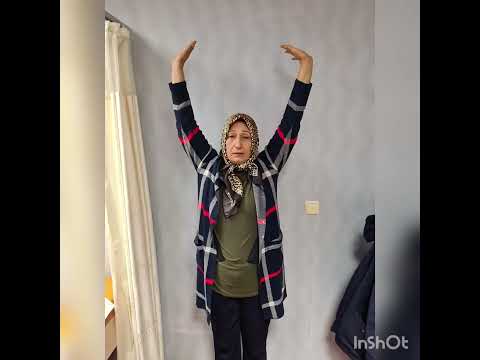
The patient did not receive any adjuvant therapy after the surgery. She had
been fol[1]lowed
up for seven months with no sign of recurrence and pain (Figure 2B).
Discussion
Schwannomas
are the most common tumors derived from schwann cells of nerve fibers.
Intraosseous schwannoma, however, is very rare, accounting for less than one
per-cent of all benign bone tumors.1-8 In addition to the sacrum, iliac wing
and mandible, intraosseous schwannomas also occur in the long bones, vertebra,
fibula and frontal bone,1-5,8 however, there is no case in literature
intraosseous schwannoma of hamate bone. Schwannomas may involve bone tissue via
three mechanisms: i) they may be intramedullary, producing rarefac[1]tion
of the bone; ii) they may be located within the nutrient canal, with the
formation of a dumbbell-shaped tumor; or iii) they may be extraosseous, eroding
into the bone.1,6,7 On the base of imaging, intraoper[1]ative findings of
dumbbell-shaped tumor inside and outside the hamate bone and gross examination,
this case demonstrates an example of intraosseous schwannoma. Intraosseous
schwannomas have char[1]acteristic
radiographic features such as a well-defined lytic lesion, sclerotic margins,
narrow transition zone, lobulated contours, cortical expansions and absence of
central calcification. However, all these radi[1]ographic findings are
non-spesific and does not help clinicians in differential diagnosis. On the
basis of CT and direct X- ray, It is difficult to differentiate the
intraosseous schwannoma from other lytic benign bone lesions of such simple
bone cyst, aneurys[1]mal
bone cyst, and giant cell tumor of bone, fibrous dysplasia, enchondroma and non[1]ossifying
fibroma. On MRI, shwannomas are solid lesions contrary to simple bone cyts and
aneurysmal bone cyts. T2 hyperin[1]tensity
of the schwannomas can be bright as much as that of enchondroma. However,
enhcondromas may contain calcifications with typical contrast enhancing views
on MRI. Giant cell tumors, fibrous dysplasia and non-ossiying fibromas are
heteroge[1]nous
tumors having both T2 hyper and hypointense areas. On CT, giant cell tumors
have lytic borders due to its local agresive-
ness
and fibrous dysplasias have ground[1]glass
apperance with wide transition zone. CT and MRI scans in our case showed that
the lesion was expansile with cortical break-through and extra osseous
extension but well defined borders within both bone and soft tissues. The
sclerotic, well-defined borders have narrow transition zone on CT and plain
radiography. These findings may be the characteristic for intraosseous
schwannomas.1-4,7,8 The final diagnosis of intraosseous schwannoma was made by
his[1]tologic
examination of tumor. The histolog[1]ic
features of this lesion are similar to those of soft tissue schwannoma.
Conclusions
Making
diagnosis of an intraosseous schwannoma pre-operatively with clinical and
radiological findings, and needle biopsy was beneficial to the patient to avoid
unnecessary adjuvant therapy. Surgical excision is the pre[1]ferred
treatment option. If significant bony defect occurs, bone grafting should be
consid[1]ered.
These tumors are generally well encapsu[1]lated
without invasion of the surrounding struc[1]tures, enabling complete
resection possible. Recurrence is rare after complete resection.
 لغة
لغة Türkçe
Türkçe English
English Arabic
Arabic Germany
Germany Russian
Russian