Popliteal Fossa Sarcomas
Sarkomy popliteální fossy
O. ERDOGAN 1, A. ÇELİK 2, A. N. T. YILDIRIM 3, E. TEKÇE 4, G. ALTUN 5, S.
DEMİRÖZ 6, Y. GÜLER 8, K. OZKAN 2, V. GURKAN 7
-
Haydarpasa Numune Training and Research Hospital, Orthopaedics and
Traumatology Clinic, Istanbul, Turkey
-
Istanbul Medeniyet University, Faculty of Medicine, Orthopaedics and
Traumatology Clinic, Istanbul, Turkey
-
Istanbul Medeniyet University, Faculty of Medicine, Pathology Clinic,
Istanbul, Turkey
-
Bezmialem University, Faculty of Medicine, Radiation Oncology Clinic,
Istanbul, Turkey
-
Ümraniye Training and Research Hospital, Orthopaedics and Traumatology
Clinic, Istanbul, Turkey
-
Kocaeli University, Orthopaedics and Traumatology Clinic, Kocaeli, Turkey
-
Bezmialem University, Faculty of Medicine, Orthopaedics and Traumatology
Clinic, Istanbul, Turkey
-
Baltalimanı Training and Research Hospital, Orthopaedics and Traumatology
Clinic, Istanbul, Turkey
ABSTRACT
PURPOSE OF THE STUDY
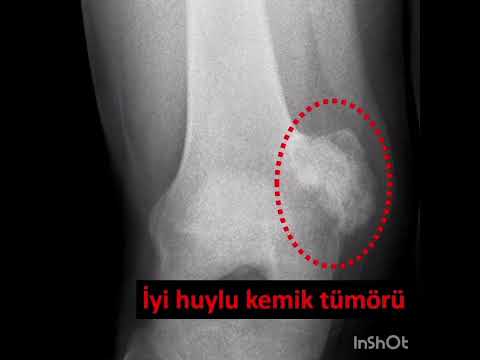
Soft tissue sarcomas of the popliteal fossa are extremely rare tumors of
mesenchymal origin accounting for 3%–5% of all
extremity sarcomas. However, data regarding the tumor type, neurovascular
involvement, and administration of radiation
therapy before or after resection are limited. This study aimed to report on
popliteal fossa sarcomas analyzing data from two
institutions based on a relatively large patient sample.
MATERIAL AND METHODS
Twenty-four patients (80%; 9 men and 15 women) with a popliteal fossa soft
tissue sarcoma were included in this study.
The reviewed patient data included sex, age, duration of complaints, interval
to diagnosis, radiology, pre- and postoperative
biopsy, tumor histology, surgery type, complications, and pre- and
postoperative oncologic and functional outcomes. The
minimum follow-up was 24 months.
RESULTS
The mean age of the patients was 48 ± 21.23 (range 3–72) years at the time of
diagnosis. The mean follow-up was
41.79 ± 16.97 (range 24–120) months. The most common histological diagnoses
were synovial sarcoma (6 patients), hemangiopericytoma (2 patients), soft
tissue osteosarcoma (2 patients), unidentified fusiform cell sarcoma (2
patients), and
myxofibrosarcoma (2 patients). Local recurrence after limb salvage was
observed in six patients (26%). At the latest followup, 2 patients died of the
disease, 2 patients were still alive with progressive lung disease and soft
tissue metastasis, and
the remaining 20 patients were free from the disease.
CONCLUSIONS
Microscopically positive margins may not be an absolute indication for
amputation. Also, negative margins do not provide
a guarantee that local recurrence will not occur. Lymph node or distant
metastasis may be predictive factors for local
recurrence rather than positive margins.
Key words: fossa poplitea, sarcoma.
INTRODUCTION
Soft tissue sarcomas of the popliteal fossa are extremely rare tumors of
mesenchymal origin, accounting for 3%–5% of all extremity sarcomas (6, 17).
The popliteal fossa region includes major structures such as popliteal vessels
and posterior tibial and common peroneal nerves. Also, tumors are
extracompartmental because of no barrier and may require extensive
neurovascular reconstructions; therefore, they have a worse prognosis (8).
(Soft tissue transfers may also be required in large tumors with skin invasion
(13). Advances in staging and limb-salvaging procedures and the use of
radio-chemotherapy reduced amputation rates. Local micro-spread can be
decreased by neoadjuvant radiation therapy, and unresectable lesions can
become resectable in some cases with a neoadjuvant chemotherapy. Sciatic nerve
sacrifice is no longer considered a contraindication for limb salvage (7).
Previous reports argued that survival is directly affected by tumor size and
grade (12, 13). However, data regarding the tumor type, neurovascular
involvement, and the time of administration of radiation therapy are limited.
Also, most of the studies on popliteal fossa sarcomas were based on small
patient cohorts. In this study, the clinical aspects such as presentation and
postoperative complications were evaluated. The local recurrence, metastasis,
amputation and limb salvage rates were also investigated according to the
tumor type, grade, size, neurovascular involvement, neoadjuvant therapies, and
surgical techniques. This study aimed to report on popliteal fossa sarcomas
using data from two institutions based on a relatively large patient sample.
MATERIAL AND METHODS
The study was performed in accordance with the ethical standards of the
Declaration of Helsinki. All patients provided informed consent before
inclusion in the study, and a local ethics committee approved the study
protocol. The present retrospective study consists of 24 surgically treated
popliteal fossa tumor from January 2003 to December 2018. A manual search of
the operating room records of senior surgeons was performed for the terms
“soft tissue tumor,” “sarcoma,” and “popliteal fossa.” Of the 30 patients, 24
(80%; 9 men and 15 women) with soft tissue sarcoma were included in the
present study. The reviewed patient data included gender, age, duration of
complaints, interval to diagnosis, radiology, pre- and postoperative biopsy,
tumor histology, surgery type, complications, and pre- and postoperative
oncologic and functional outcomes. Eligibility criteria included patients
having popliteal sarcomas, with a minimum follow-up of 2 years for survivors.
For other patients, the duration of follow-up was defined by the
last-documented clinical follow-up. Nonoperated patients were excluded. All
patients were staged according to the American Joint Committee on Cancer
(AJCC). The functional scores were assessed using the Musculoskeletal Tumor
Society Score (MSTS) and the Toronto Extremity Salvage Scores (TESS). All
patients had neoadjuvant radiation therapy aiming to achieve negative surgical
margins. Only patients with metastasis received postoperative chemotherapy.
For other patients, the duration of follow-up was defined by the
last-documented clinical follow-up. The presence of neurovascular invasion was
accepted only if a pathological examination was confirmed. If the surgical
margin was >0.1 mm, it was considered intact. The popliteal fossa was
defined as proximal-medial; the semimembranosus and semitendinosus muscles and
as proximal-lateral the biceps femoris muscle. Two heads of the gastrocnemius
muscle forms the distal border. The floor consisted of posterior distal femur,
joint capsule, and popliteus muscle. Local recurrence and meta - stasis were
investigated in scheduled follow-up controls. The normality of continuous
variables were investigated by Shapiro-Wilk’s test. Descriptive statistics
were presented using mean and standard deviation, median (and
minimum-maximum). For comparison of two normally distributed groups Student t
test was used. Nonparametric statistical methods were used for values with
skewed distribution. For comparison of two non-normally distributed groups
Mann Whitney U test was used. The χ² test (Fisher’s Exact) was used for
categorical variables and expressed as observation counts (and percentages).
Statistical significance was accepted when two-sided p value was lower than
0.05. Statistical analysis was performed using the SPSS for Windows software
package (version 13.0.0; SPSS).
RESULTS
The mean age was 48 ± 21.23 (range 3–72) years. The mean follow-up was 41.79 ±
16.97 (range 24–120) months. The incidence rate of popliteal fossa sarcomas
was 1.3% in this present study. The most common dia gnoses were synovial
sarcoma (n = 6), hemangioperi - cytoma (n = 2), soft tissue osteosarcoma (n =
2), unidentified fusiform cell sarcoma (n = 2), and myxofibrosarcoma (n = 2).
One low-grade fibromyxosarcoma, one clear-cell sarcoma, one extraskeletal
chondrosarcoma and one low-grade myxoliposarcoma, one pleomorphic sarcoma, one
Ewing sarcoma metastasis, one Ewing sarcoma, and one malign schwannoma were
also identified. Two patients lesions could not be specified. All tumors
except one were primary. The median tumor size was 7.73 ± 3.19 (range 15–3.2)
cm. Lesions were low grade in 3 patients (grade I), intermediate grade (grade
2) in 3 patients, and high grade (grade 3) in 18 patients. At the time of
diagnosis, pulmonary metastasis was identified in five patients (21%), liver
metastasis in one patient (4%), lymph node metastasis in four patients (17%),
and neural invasion in six patients (25%). The AJCC stages were as follows:
three patients had stage Ib, three had stage II, six had stage IIIa, four had
stage IIIb, and eight had stage IV disease. The patients are summarized in
supplementum. Twenty-three patients encountered limbsalvaging surgery and one
patient encountered a primary above-knee amputation. Two patients with local
recurrence underwent amputation. Also, lung metastases developed in one of
them. Two deaths occurred due to synovial sarcoma and malignant peripheral
nerve shield tumor because of metastasis at diagnosis and early-term
follow-up, respectively. The mean event-free survival was 13.8 months. In one
patient, 14 months after the initial, extraarticular knee-joint resection and
prosthesis, a local recurrence was encountered with neurovascular invasion and
an above-knee amputation was conducted. In another patient, 11 months after
the initial surgery, extraarticular knee-joint resection and prosthesis were
done, and a local recurrence was encountered. After two unsuccessful revision
surgeries, a hip disarticulation was conducted. Limp sparing rate was 87.5% in
this present study. Surgical margins were negative in 20 patients and
microscopically positive in 4 patients. All residual diseases were treated
with wide local ‘’surgical bed’’ excisions. Chemotherapy was administered in
eight patients (preoperatively in one, postoperatively in two, and both pre-
and postoperatively in five patients). Neoadjuvant chemotherapy was intended
to shrink the mass and provide a limb salvage in four patients. These patients
had unresectable masses. Absent of response in one patient caused to
amputation. Radiotherapy was administered in 14 patients, postoperatively in 6
patients (63 Gy) and preoperatively in 8 patients (50 Gy). All high-grade
tumors except amputated patients underwent radiotherapy. Sciatic nerve
branches in four patients, common peroneal nerve in two patients, deep
peroneal nerve in one patient, and common peroneal and tibial nerve in one
patient were resected. Local recurrence after limb salvage was recorded in six
patients (26%). Only in one of them, the surgical margins were positive. In
four of this six patients, lymph node metastasis was detected. In this regard,
lymph node or distant metastasis might be predictive
Table 1. Preferences of patients with local recurrences
|
Tumor type
|
Grade
|
At diagnosis
|
Margins
|
Administered adjuvant treatment
|
|
Hemangioapericytoma
|
3
|
neurovascular invasion
|
positive
|
post op chemotherapy
|
|
Clear-cell sarcoma
|
3
|
lymph node, liver metastasis
|
negative
|
pre op radiotherapy
|
|
Synovial sarcoma
|
3
|
no metastasis
|
negative
|
pre–post op radiotherapy
|
|
Chondrosarcoma
|
2
|
lymph node metastasis
|
negative
|
pre–post op chemotherapy post op radiotheraphy
|
|
Ewing sarcoma metastasis
|
3
|
lymph node lung metastasis
|
negative
|
none
|
|
Osteosarcoma
|
3
|
lymph node, liver metastasis
|
negative
|
pre–post op chemotheraphy
|
factors for a local recurrence. However, we could not compare lymph node
positivity and margin positivity in terms of local recurrence risk, since the
number of patients with margin positivity was only one in our series.
Preferences of patients with local recurrence are given in Table 1. Lung
metastasis developed in nine patients (38%) and liver metastasis in two (8%)
after treatment. In this study, the rate of metastatic disease at diagnosis
was 42%. The amputation rate was 13%, the local recurrence rate was 26%, the
total complication rate was 29%, and the wound complication rate was 25%.
However, there was no correlation between the metastasis at presentation and
local recurrence in our series. Details on tumor type, metastasis site,
metastasis time and treatment are given in Table 2. Postoperative
complications included wound dehiscence in three patients. Postoperative
radiotherapy regimen in one of them and preoperative radiotherapy regimens in
two of them were used (Fig. 1). None required soft tissue reconstruction. No
clinical signs of deep vein thrombosis were detected in any of the patients in
the present series. In a 3-year-old patient, a femur fracture was encountered
after 3 months from the initial surgery due to excessive periosteal stripping.
Union was achieved with an elastic nail fixation. The MSTS score was evaluated
in 22 patients, and the mean score was 81.2 (range 65.0–92.5). The TESS was
evaluated in 22 patients, and the mean result was 77.4 (range 67.2–95). The
worst result belonged to a patient who had an intralesional resection in
another center. Postoperative radiotherapy at 66 Gy and wide re-resection were
performed for this patient. No local recurrence was encountered in 2 years,
but the patient died after the latter surgery because of multiple visceral
metastasis (Fig. 2–3). The local recurrence rate was 6/23 (26%), and the
mean recurrence time was 8.8 ± 2.3 months. The visceral metastasis rate was
9/24 (36%), and the mean time was 10.11 ± 3.2 months. In the present study,
five neural and eight vascular invasions were detected. Of the 20 patients
with neurovascular stripping, only 5 (25%) had a local recurrence. Of the six
patients with local recurrence, four patients had no pre-/postoperative
radiotherapy. We could not detect a relationship between the type of adjuvant
treatment and the risk of local recurrence because the adjuvant treatment
types in our series were not homogeneous and the case number was limited. Two
patients needed amputation (above-knee and hip disarticulation) after limb
salvage because of local recurrence. At the latest follow-up, two patients
died of the disease, another two patients were still alive with progressive
lung disease and soft tissue metastasis, and the remaining 20 patients were
free from the disease.
DISCUSSION
Soft tissue sarcomas of the popliteal fossa are extremely rare tumors of
mesenchymal origin accounting for 3%–5% of all extremity sarcomas. Turcotte et
al. reported this rate as 2.7% in their series (17). In the present sarcoma
series, the incidence rate of popliteal fossa sarcomas was close to these
results (1.3%). Recent studies showed that the use of radio-chemotherapy could
produce limb-sparing rates of 65%–95% (2, 4) and similar results were obtained
in the present cohort (87.5%). Surgical margins are one of the most important
factors affecting local recurrence (18). In this study, the adventitia or the
nerve sheath was routinely removed when the vessels or nerve was in close
proximity. In a recent study authors reported that although the close
proximity, vital
Table 2. Tumor type, metastasis site, metastasis time, and treatment
|
Tumor type
|
Metastasis site
|
Metastasis time (month)
|
Treatment
|
|
Hemangiopericytoma
|
lung
|
6
|
lobectomy + chemotherapy
|
|
Low differantiated. synovial sarcoma
|
lung
|
9
|
surgery + chemotherapy
|
|
Soft tissue osteosarcoma
|
lung (bilateral)
|
0
|
surgery + chemotherapy
|
|
Clear-cell sarcoma
|
liver + lung
|
0/36
|
pazopanib 800 mg tablet (once a day)
|
|
Synovial sarcoma
|
liver
|
24
|
died because of metastasis
|
|
Unidentified fusiform cell sarcoma
|
lung
|
11
|
lobectomy/lymph node excision + chemotherapy
|
|
Synovial sarcoma
|
lung
|
9
|
lobectomy + chemotheraphy
|
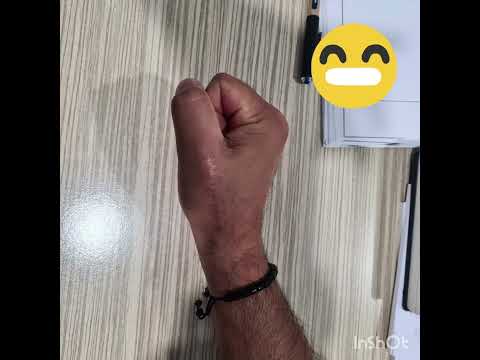
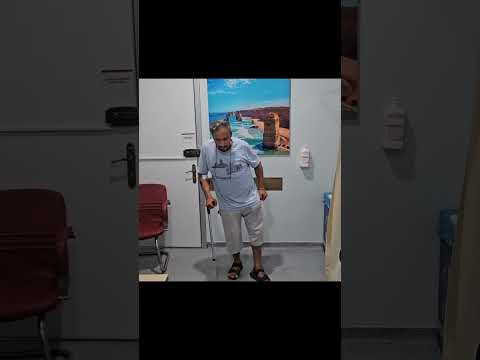
Fig. 1. A popliteal “S’’ incision (a). Neurovascular stripping from the
tumor (b). After the resection, some dead space was present (c). A myxoid
liposarcoma (d).
tissues were surrounded by the tumor only in 11.5%. They concluded that
carcinomas infiltrate, sarcomas displace the vessel and nerve (5). Negative
margins plus radiotherapy provide lower rates of local recurrence (14).
Radiation therapy has been reported as an adjuvant that improves the local
recurrence rates (11). However, radiotherapy is unable to control the positive
margins. We could not detect a relationship between the type of adjuvant
treatment and the risk of local recurrence because the adjuvant treatment
types in our series were not homogeneous and the case number was limited.
Local recurrences after popliteal soft tissue tumors are usually encountered
within 2 years after the initial procedure (3). In this series, in patients
with local recurrence, lymph node metastasis rate was high. Thus, lymph node
metastasis might be predictive factor for a local recurrence. However, we
could not compare lymph node positivity and margin positivity in terms of
local recurrence risk, since the number of patients with margin positivity was
only one in our series. Turcotte et al. reported the recurrence rate of
positive margin as 9% (1/11) in their series of 18 patients. In the present
series, only one patient had positive margins, who had a local recurrence. The
relationship between local recurrence and survival remains unclear.
Pritsch et al reported a series of 27 cases. They reported that 7% of patients
had metastatic disease at diagnosis. The amputation rate was 14%. They also
reported no difference between the amputees and the limb-salvage group
according to survival (12). The rate of local recurrence was 10% and the wound
complication rate was 30%, in their series. In this present study, in
five-sixth of local recurrence cases, surgical margins were negative. This
result was attributed to the fact that the surgical margins <1 mm were
accepted as intact. Neoadjuvant radiotherapy had a negative impact on wound
tissue healing (15). Also, radiation-induced fibrosis, lymphedema, and joint
stiffness might alter the functional scores (1, 16). In this study, no
relationship was found between neoadjuvant-adjuvant radiotherapy and wound
complications/lower functional scores (Mann-Whitney U p=0.857). Adjuvant
radiotherapy may has more effect on functional scores compared to neo-adjuvant
radiotherapy and this effect may increase as follow-up time increases.
However, we could not find any correlations between adjuvant radiotherapy and
functional scores (Spearman’s rho correlation p=0.097). Wound complications
might alter the functional scores. However, in this study, no complications
were encountered in a patient in whom the

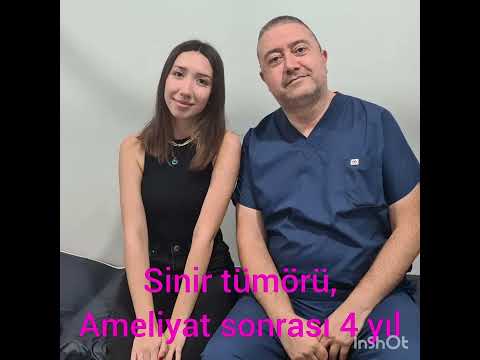
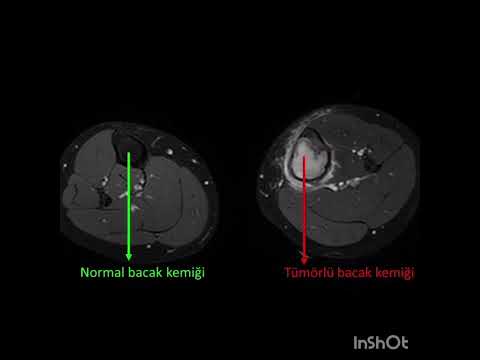
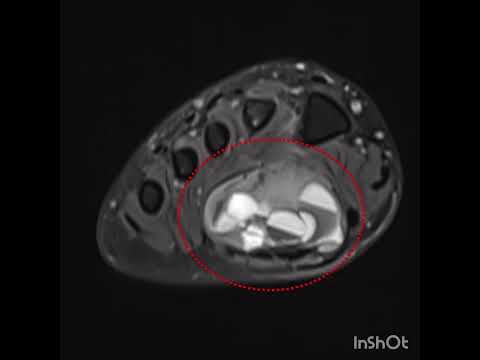
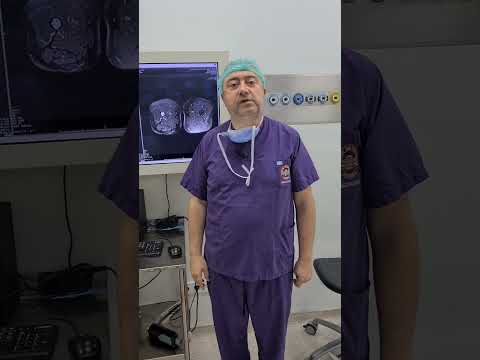
Fig. 2. Axial MRI of a popliteal tumor (a). Skin incision that included the
biopsy tract (b). Neurovascular stripping from the tumor (c). Tumor and
neurovascular bundle proximity (d).
medial hamstring and medial head of the biceps muscle with neoadjuvant
radiotherapy were resected. In another patient, the gastrocnemious lateral
head was resected, and no complications were encountered. In two other
patients, the posteromedial corner reconstruction with allograft and
rotational gastrocnemious flap was made with postoperative radiotherapy. No
complications were encountered, and the mean TESS score was 85 in these two
patients. Turcotte et al. reported the TESS and MSTS 1987 mean scores as 82.4%
and 33/35, respectively. Bickels et al. reported 15 patients who underwent
sciatic nerve resection. They reported good functional results (17). In our
study, the sacrificed nerve branches of the sciatic nerve did not reduce the
functional results. There were four patients with sciatic nerve resection.
There was no significant difference between them and those who did not undergo
nerve resection in terms of TESS and MSTS scores. This result may be due to
the lack of sufficient patients who underwent resection. Radiotherapy was
applied to 13 patients before or after surgery. No significant effect of
radiotherapy on TESS and MSTS scores was found. All below-average functional
scores and local recurrences might belong to neurovascular stripping. Also,
amputation, multiple metastases, and fracture might belong to lower scores.
Data regarding detailed analysis of neurovascular involvement are limited.
Four neural resections and three vascular by-passes were performed. Only in
two patients who underwent neurovascular stripping (margins < 1 mm), local
recurrence was detected. Hohenberger et al. reported 20 patients with soft
tissue sarcoma invading neurovascular structures, but only four patients had
popliteal fossa tumors (9). No other study has evaluated neurovascular
involvement so far. The present study had several limitations. It was a
retrospective study and was relatively small and heterogeneous. Second, the
minimum follow-up was only 2 years. However, to our knowledge, this report is
one of the largest series about popliteal soft tissue sarcomas in English
literature. The rates of local recurrence and systemic disease increased only
slightly during a longer follow-up because local recurrence and metastasis
usually occur in first two years, and the median follow-up in this study was
more than 70 months (5). The hyperthermic isolated limb perfusion method is a
technique that provides intense anti-cancer drug delivery to the tumor region
with less systemic effects. Neo or adjuvant application of this method may be
useful in convert of an unresectable mass to a resectable mass (10).


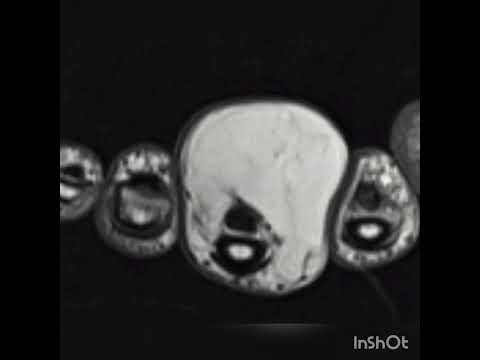
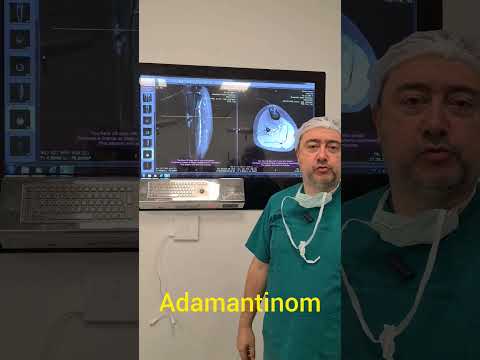
Figure 3. After the excision (a). A myxofibrosarcoma (b). Low-power
histogram (c). High-power histogram (d).
CONCLUSIONS
In conclusion, microscopically positive margins may not be an absolute
indication for amputation. Also, negative margins do not provide a guarantee
that local recurrence will not occur. Lymph node or distant metastases may be
predictive factors for local recurrence rather than positive margins.
Therefore, in these patients, preoperative radiotherapy was suggested despite
wound complication risk.
Ethics approval and consent to participate: This study was approved by the
local ethical committee and informed consent has been taken from all
participants. Availability of data and materials: The datasets used and/or
analysed during the current study are available from the corresponding
author on reasonable request. All authors read and approved the final
manuscript.
References
-
Avraham T, Yan A, Zampell JC, Daluvoy SV, Haimovitz-Friedman A, Cordeiro AP,
Mehrara BJ. Radiation therapy causes loss of dermal lymphatic vessels and
interferes with lymphatic function by TGF-beta1-mediated tissue fibrosis. Am
J Physiol Cell Physiol. 2010;299:C589–605.
-
Bell RS, O’Sullivan B, Liu FF, Powell J, Langer F, Fornasier VL, Cummings B,
Miceli PN, Hawkins N, Quirt I. The surgical margin in soft tissue sarcoma. J
Bone Joint Surg Am. 1989;71:370–375.
-
Cantin J, McNerr GP, Chu FC, Booher RJ. The problem of local recurrence
after treatment of soft tissue sarcoma. Ann Surg. 1968;168:47–53.
-
Cormier JN, Ballo MT. The influence of anatomic location on functional
outcome in lower-extremity soft-tissue sarcoma (comment). Ann Surg Oncol.
2004;11:453–454.
-
Davis AM, O’Sullivan B, Turcotte R, Bell R, Catton C, Chabot P, Wunder J,
Hammond A, Benk V, Kandel R, Goddard K, Freeman C, Sadura A, Zee B, Day A,
Tu D, Pater J; Canadian Sarcoma Group; NCI Canada Clinical Trial Group
Randomized Trial. Late radiation morbidity following randomization to
preoperarive versus postoperative radiotherapy in extremity soft tissue
sarcoma. Radiother Oncol. 2005;75:48–53.
-
Eilber FC, Eckardt JJ, Rosen G, Nelson SD, Selch M, Eilber FR. Large, deep,
high-grade extremity sarcomas: treating tumors of the flexor fossae. Surg
Oncol. 1999;8:211–214.
-
Eilber FR, Eckardt JJ, Rosen G, Fu YS, Seeger LL, Selch MT. Neoadjuvant
chemotherapy and radiotherapy in the multidisciplinary management of
soft-tissue sarcomas of the extremity. Surg Oncol Clin North Am.
1993;2:611–620.
-
Enneking WF. A system of grading musculoskeletal neoplasms. Clin Orthop
Relat Res. 1986;204:9–24.
-
Hohenberger P, Wysocki WM. Neoadjuvant treatment of locally advanced soft
tissue sarcoma of the limbs: which treatment to choose? Oncologist.
2008;13:175–186.
-
Lesenský J, Vočka M, Špaček M, Hósová M. [Neoadjuvant use of ısolated limb
perfusion in large myxoid liposarcoma of the thigh: a case report]. Acta
Chir Orthop Traumatol Cech. 2021;88:321–324.
-
O’Sullivan B, Davis AM, Turcotte R, Bell R, Catton C, Chabot P, Wunder J,
Kandel R, Goddard K, Sadura A, Pater J, Zee B. Preoperative versus
postoperative radiotherapy in soft-tissue sarcoma of the limbs: a randomised
trial. Lancet 2002;359:2235–2241.
-
Pritsch T, Bickels J, Winberg T, Malawer MM. Popliteal sarcomas.
Presentation, prognosis, and limb salvage. Clin Orthop Relat Res.
2006;455:225–233.
-
Rüdiger HA, Beltrami G, Campanacci DA, Mela MM, Franchi A, Capanna R. Soft
tissue sarcomas of the popliteal fossa: outcome and risk factors. Eur J Surg
Oncol. 2007;33:512–517.
-
Shiu MH, Collin C, Hilaris BS, Nori D, Manolatos S, Anderson LL, Hajdu SI,
Lane JM, Hopfan S, Brennan MF. Limb preservation and tumor control in the
treatment of popliteal and antecubital soft tissue sarcomas. Cancer.
1986;57:1632–1639.
-
Stinson SF, DeLaney TF, Greenberg J, Yang JC, Lampert MH, Hicks JE, Venzon
D, White DE, Rosenberg SA, Glatstein EJ. Acute and long-term effects on limb
function of combined modality limb sparing therapy for extremity soft tissue
sarcoma. Int J Radiat Oncol Biol Phys. 1991;21:1493–1499.
-
Straub JM, New J, Hamilton CD, Lominska C, Shnayder Y, Thomas SM.
Radiation-induced fibrosis: mechanisms and implications for therapy. J
Cancer Res Clin Oncol. 2015;141:1985–1994.
-
Turcotte RE, Ferrone M, Isler MH, Wong C. Outcomes in patients with
popliteal sarcomas. Can J Surg. 2009;52:51–55.
-
Wilson AN, Davis A, Bell RS, O'Sullivan B, Catton C, Madadi F, Kandel R,
Fornasier VL. Local control of soft tissue sarcoma of the extremity: the
experience of a multidisciplinary sarcoma group with definitive surgery and
radiotherapy. Eur J Cancer. 1994;30A:746–751.
 Sprache
Sprache Türkçe
Türkçe English
English Arabic
Arabic Germany
Germany Russian
Russian